
Museums represent the legacy of the past, focusing upon artifacts that connect us to this past. A museum has three fundamental purposes: the curation and maintenance of artifacts that preserve and promote history, fostering remembrance of the past and its heritage, and research. All center upon information and teaching which are linked today by digital technologies. Yet the artifacts themselves are not digital. Written words, digital images, podcasts, videos, motion pictures, and other electronic presentations can capture the spirit of the object, but they are not the object itself. Museums with intrinsically-valuable artifacts may always endure, but such treasures run the risk of destruction and require preservation.
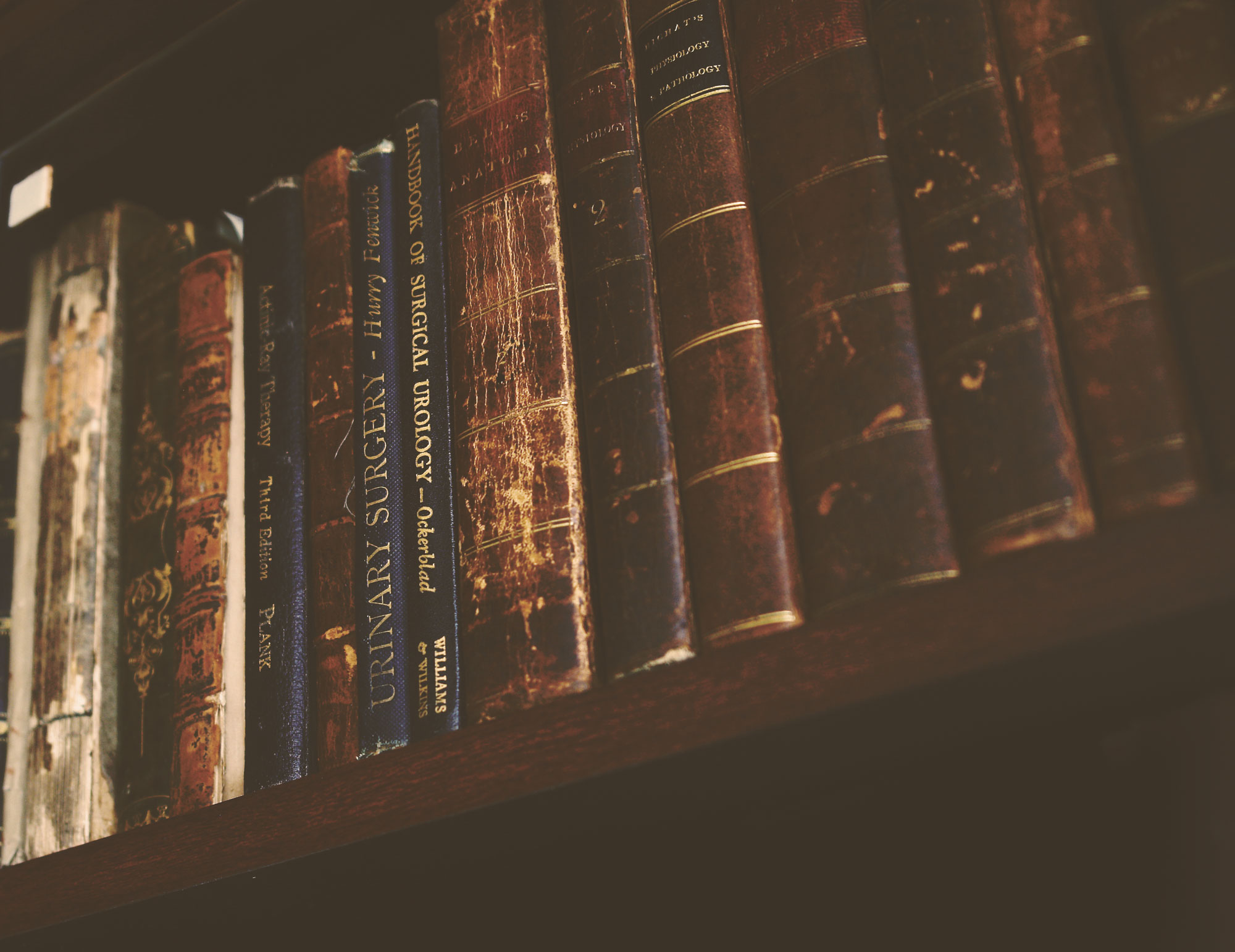
The history of medicine and the history of urology is vitally important to our specialty. Armed and educated with the knowledge of past contributions that led to future advancements, our members and trainees are better equipped to treat and to teach. In addition to the medical advances over the centuries, our specialty is also very dependent upon the advances in instrumentation. Seeing, touching, examining instruments and artifacts, reading about them from original sources, and researching various aspects of urology makes the preservation and display of artifacts an exceedingly valuable resource.


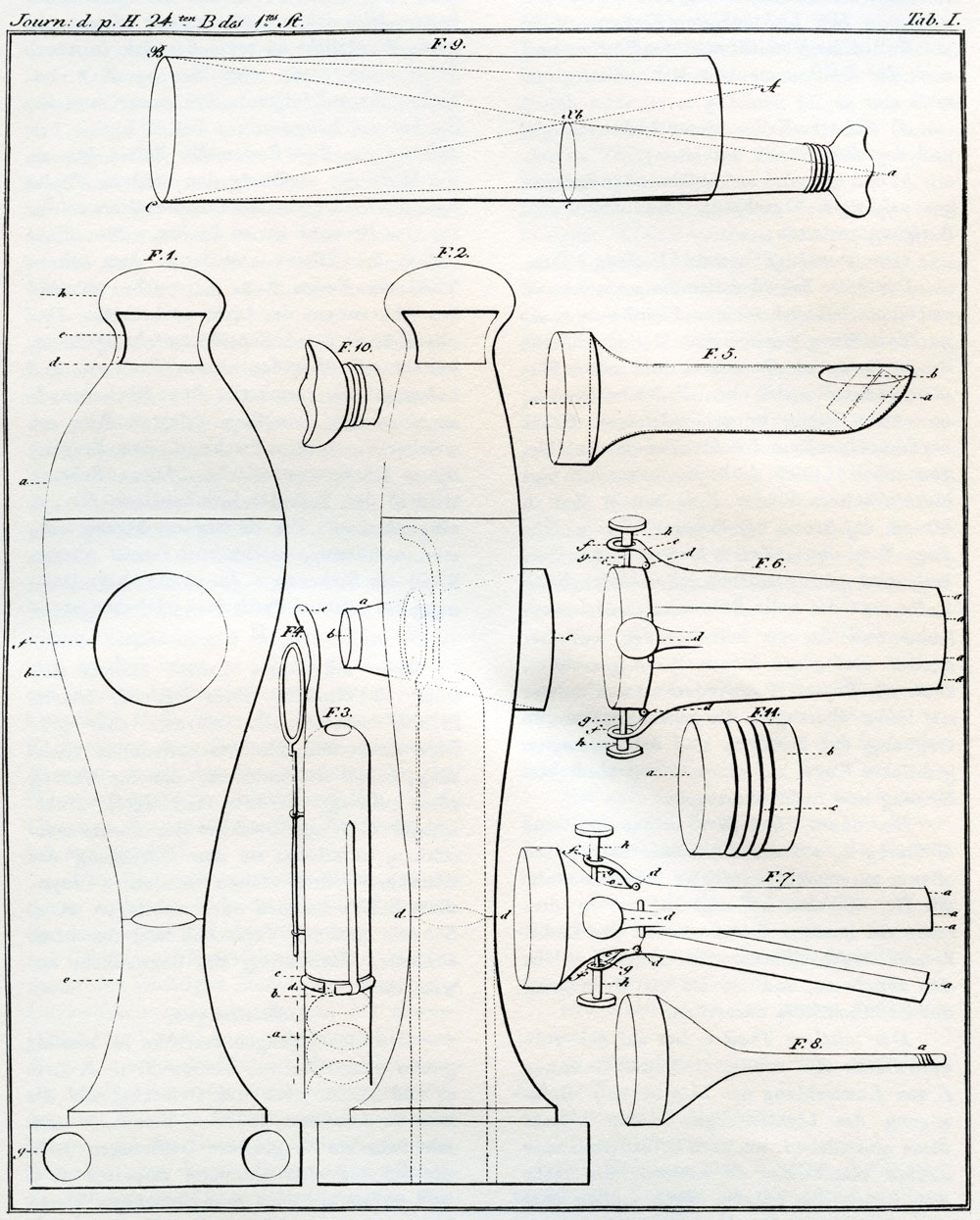
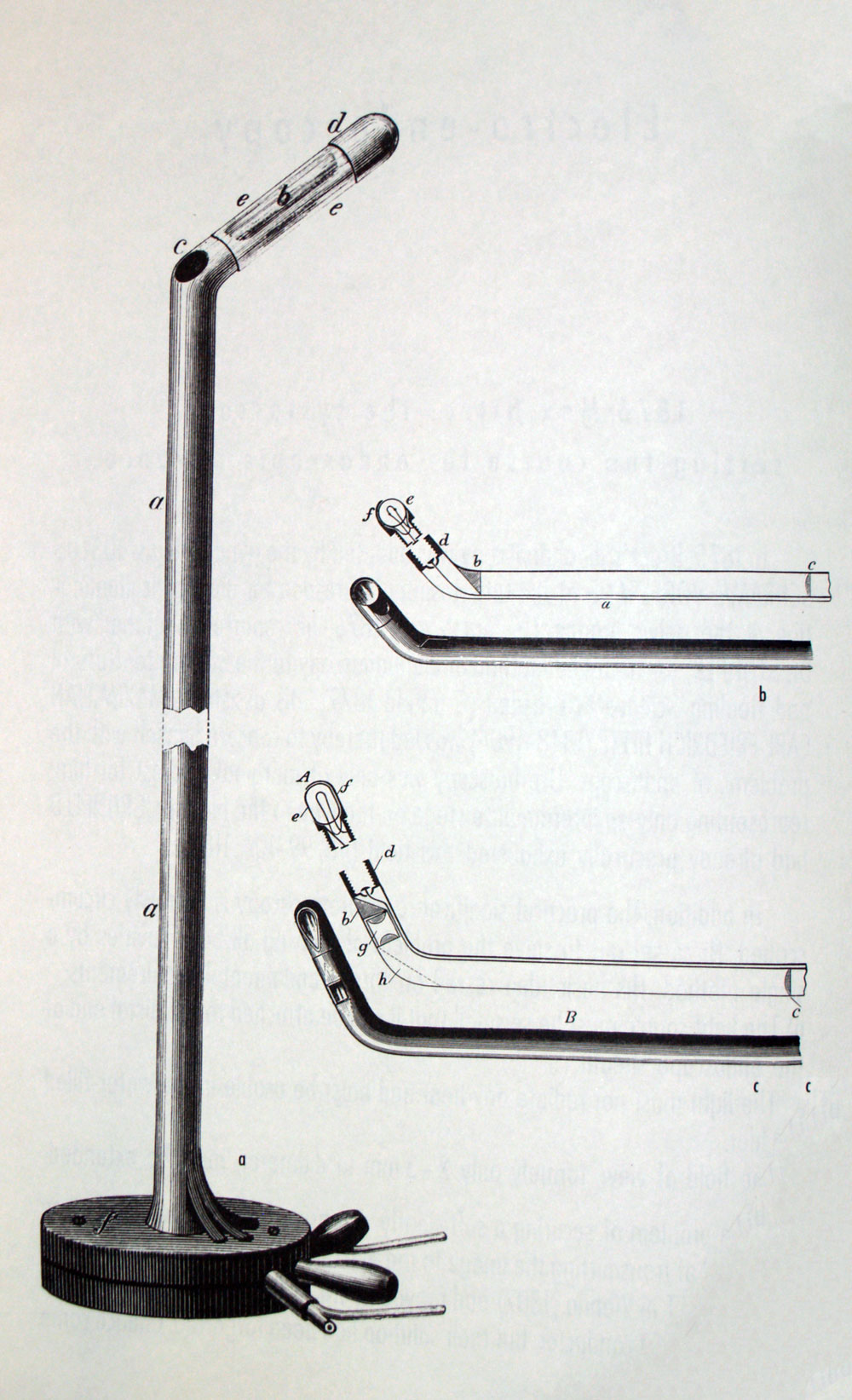
Light allows the physician to peer into the interstices of body cavities, with organs and organ systems. The hope for an endoscopic method actually began when waxed candles and mirrors provided the illumination for the first endoscope by Bozzini.
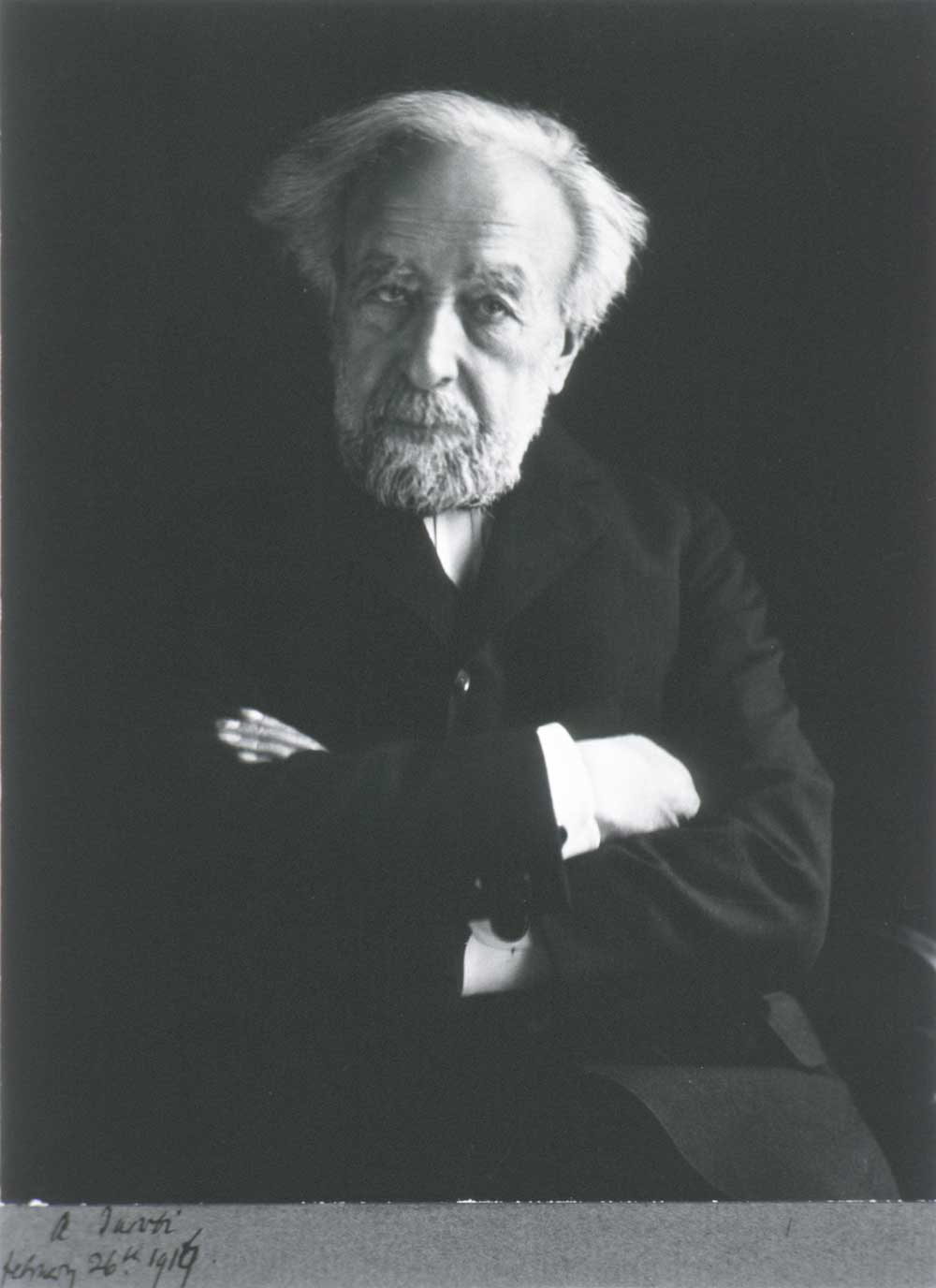
In 1805 Phillip Bozzini (1773-1809) constructed an instrument called “lichtleiter” (light carrier) for the viewing of the openings in the human body. Bozzini’s insight into the potential for direct visualization of the body is as amazing as the harsh criticism of his peers regarding his endoscopic adventures with his device. Bozzini’s light carrier consisted of a housing in which a candle was placed. Open tubes of various sizes and configurations could be placed on one side. He then devised a reflecting mirror between the visual tract and the candle light, so that the light would be reflected only toward the targeted organ and not backward into the examiner’s eye. The opposite side of the system was the eyepiece.
This development was remarkable in that it was the first use of reflected light as an illumination source. More than one of the founding fathers of the specialty of urology declared that this new and burgeoning technology was the founding stone of the specialty. It is now difficult as a urologist to even imagine a time when we could not visualize the bladder and have almost complete access to the upper tracts.




Man has battled urinary retention and the development of bladder stones throughout history. We have been using catheters as early as 3,000 BCE to relieve urinary retention.
Early catheters were made from multiple materials that allowed a hollow tube to be placed through the urethra, ranging from natural materials such as straw, reeds, hollow stalks of spring onions (Allium fistulosum) or carved wooden tubes to the use of malleable metals such as gold, silver, copper, brass and lead.
Malleable catheters were developed and silver was commonly used as it was easily malleable to further navigate the urethra or obstructing prostate in men and was felt to have antiseptic properties. An S-shaped silver tube used for the treatment of urinary retention was found during the excavation of Pompeii.


One such variation involves one of the United States’ founding fathers, Benjamin Franklin, author, printer and inventor, who fashioned a silver coil catheter for his brother who suffered from bladder stones.
Franklin worked with his local silversmith on the design for a flexible silver catheter. In a letter to his older brother John on December 8th, 1752, Franklin wrote:
Dear Brother, Reflecting yesterday on your desire to have a flexible catheter, a thought struck into my mind, how one might probably be made... I went immediately to the silversmith’s and gave directions for making one (sitting by till it was finished) that it might be ready for this post... It is as flexible as would be expected in a thing of the kind, and I imagine will readily comply with the turns of the passage, yet has stiffness enough to be protruded...
Franklin would likely use it later on himself remarking that “when I consider how many terrible diseases the human body is liable to, Icomfort myself that only three incurable diseases have fallen to my share... the gout, the stone, and old age.”
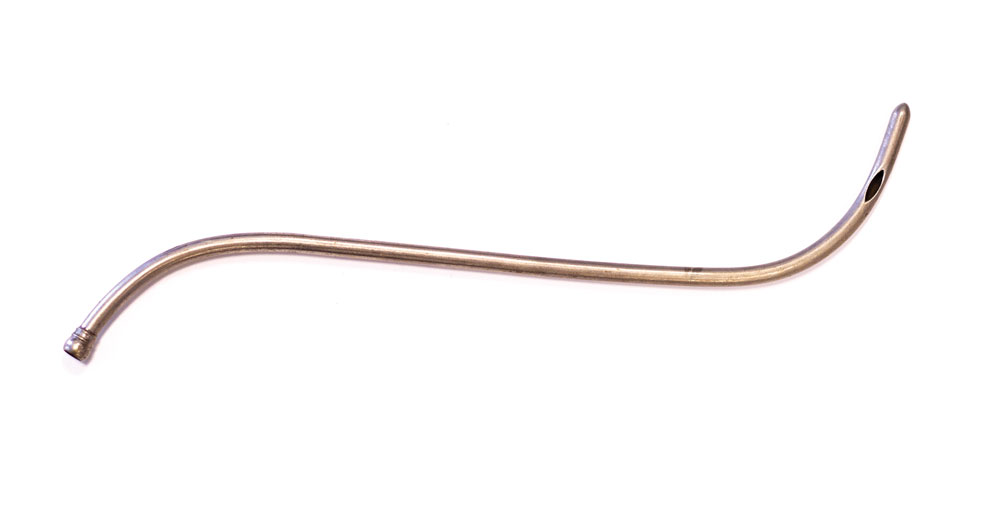


The catheter was used to help empty the bladder of thosesuffering from bladder stones and urinary retention. As bladderstones could obstruct the bladder neck making it painful tourinate, the catheter would bypass the obstruction and drain thefilled and obstructed bladder.
A constant reservoir of undrained urine due to urinaryobstruction over many years could lead to the formation of alarge stone. This impressive stone bears witness to this processand was the result of obstruction in an ideal conduit.
10 pound bladder stone, donated by Tim Roddy, MD, 2010

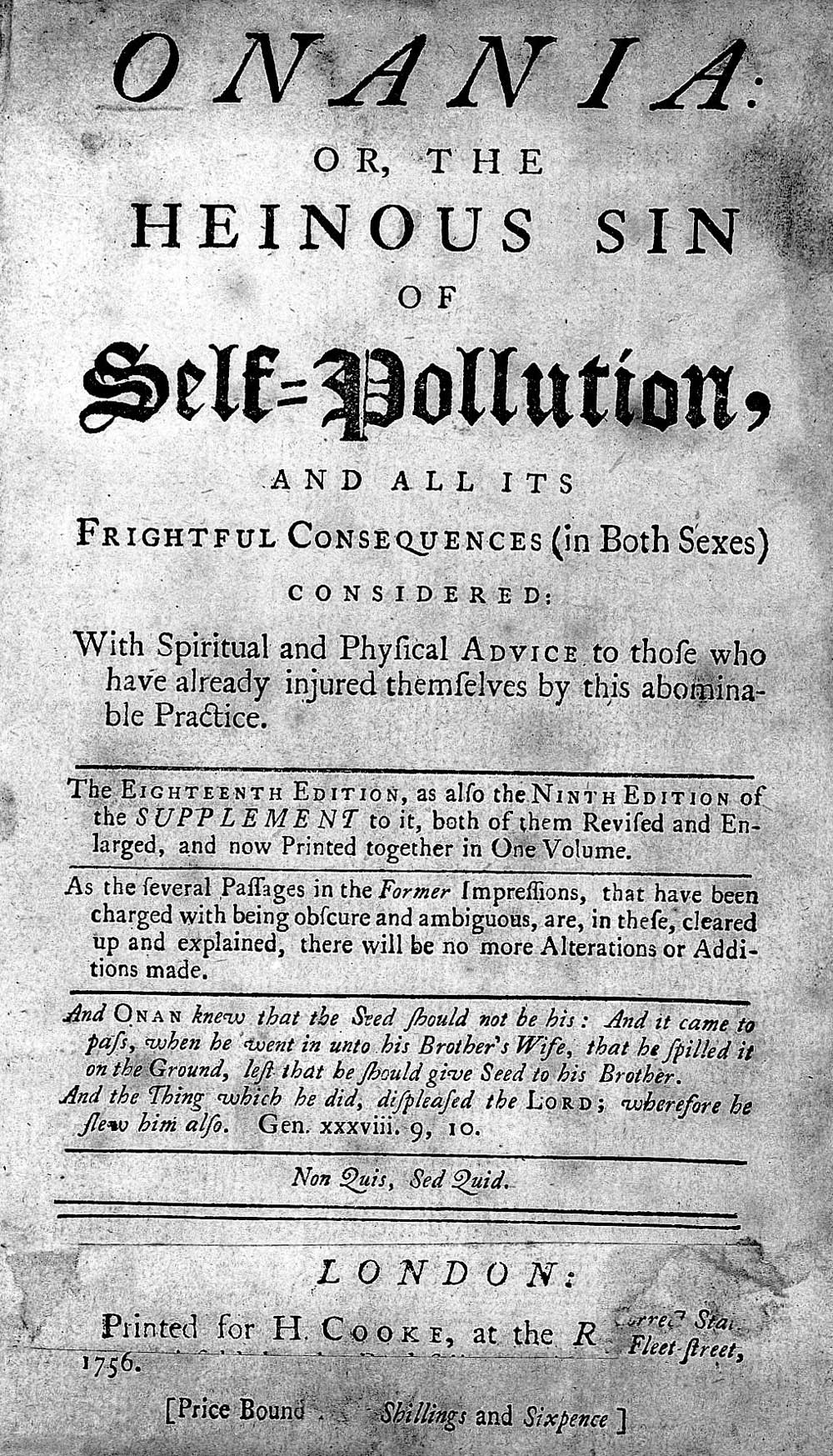
In 1715, a brochure was published in England about masturbation (onanism) entitled “Onania, or the Heinous Sin of Self-Pollution, and all its Frightful Consequences in both Sexes Considered, with Spiritual and Physical Advice to those who have already Injured Themselves by this Abominable Practice.”
In 1758, the Swiss physician Samuel Auguste Tissot (1728-1797) first published his treatise in Latin and two years later in French about the perils of masturbation, claiming that it was worse than smallpox, depleting the body of vital energies. Christophe-Guillaume Hufeland, famed Professor at the University of Berlin, and physician to Schiller, Goethe, and the King of Prussia, wrote in 1798 that masturbation was the practice most likely to shorten one’s life. The great American physician Benjamin Rush listed the terrible consequences of masturbation in 1812 including “... Impotence, dysury, tabes dorsalis, pulmonary consumption, dyspepsia, dimness of sight, vertigo, epilepsy, hypochondriasis, loss of memory, manalgia, fatuity, and death.”
Numerous publications warned about the dangers of masturbation as well as spermatorrhea (nocturnal emissions), including seizures, tuberculosis, visual impairment, heart disease, insanity, and suicide.
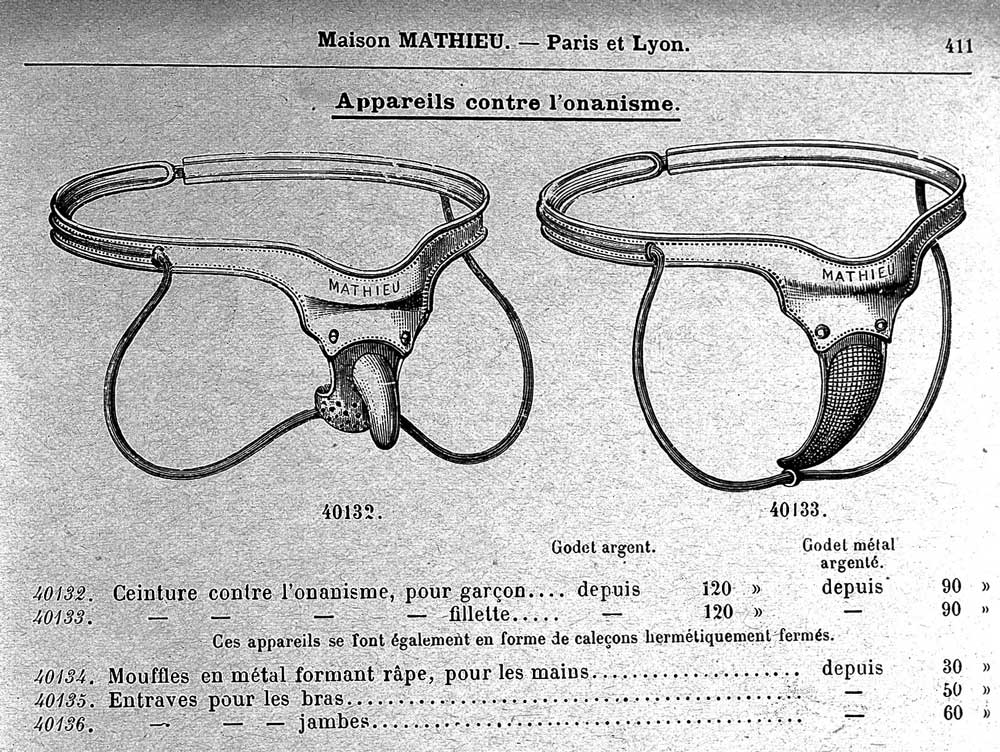
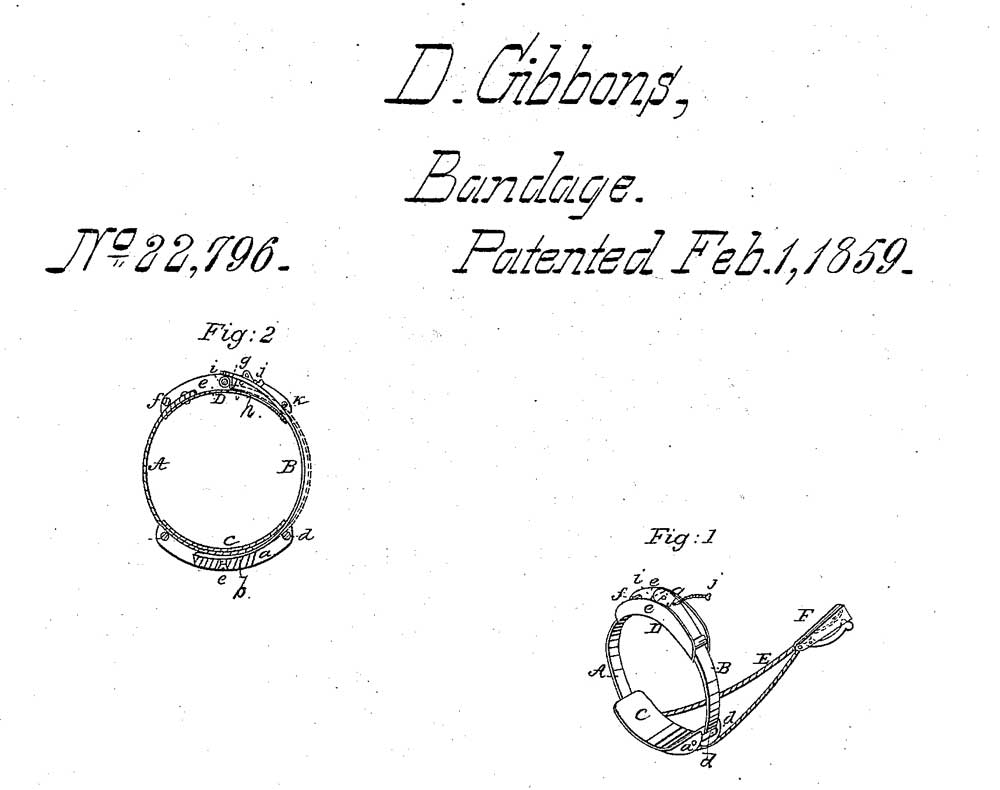
Many devices were invented to prevent erections, including rigid sheaths and sheaths clipped to pubic hair that would rip the hair when the penis became erect. Perhaps the most painful was the anti-masturbation or anti-spermatorrhea ring.
These consisted of an inner metal ring fitted snugly around the flaccid penis surrounded by an outer ring of sharp V-shaped spikes. With an erection, the spikes would penetrate the phallus. These devices represent an example of how an artifact can illustrate an entire social belief: the belief that masturbation is evil. They were sold by many companies and examples can be found in old Sears catalogues and Tiemann and Company catalogues.
Less painful treatments were also available and exist to this day. In the United States, Dr John Kellogg, director of the Sanitarium in Battle Creek, Michigan, believed that a fiber rich poor tasting diet would dull the urge to masturbate. With his brother, Will, he developed the anti-masturbation breakfast, Kellogg’s Corn Flakes. The Presbyterian minister Reverend Sylvester Graham, who railed against the evils of masturbation, thought that a bland diet would curb sexual urges and invented the unsweetened Graham Cracker.
As of this date, there have been no long-term studies of the success rates of anti-masturbation rings, Kellogg’s Corn Flakes, or Graham Crackers in preventing masturbation.
When Michael Faraday invented a rather crude generator using a magnet and a coil of copper wire that produced a tiny electric current it opened the door to American Thomas Edison and British scientist Joseph Swan, each of whom invented the incandescent filament light bulb in their respective countries in about 1878. Their incandescent bulbs were the first practical bulbs that would light for hours.
Maximilian Carl-Friedrich Nitze thought that for an instrument to be introduced with ease, minimal pain and relative safety, endoscopes must be smaller. His idea was to place lenses into the tubes at prescribed distances to focus the image at an ocular. In addition, his early version used a platinum wire in a glass jacket with water-cooling methods. He began clinical investigations with this cystoscope in 1877.
The Nitze cystoscope entered the urologist’s daily routine and practice when Edison’s electric bulb was miniaturized in the 1880s and became a basic detail of the first working cystoscopes.
These early cystoscopes with miniature (mignon) bulbs helped to establish urology as a specialty, since training and practice were required.


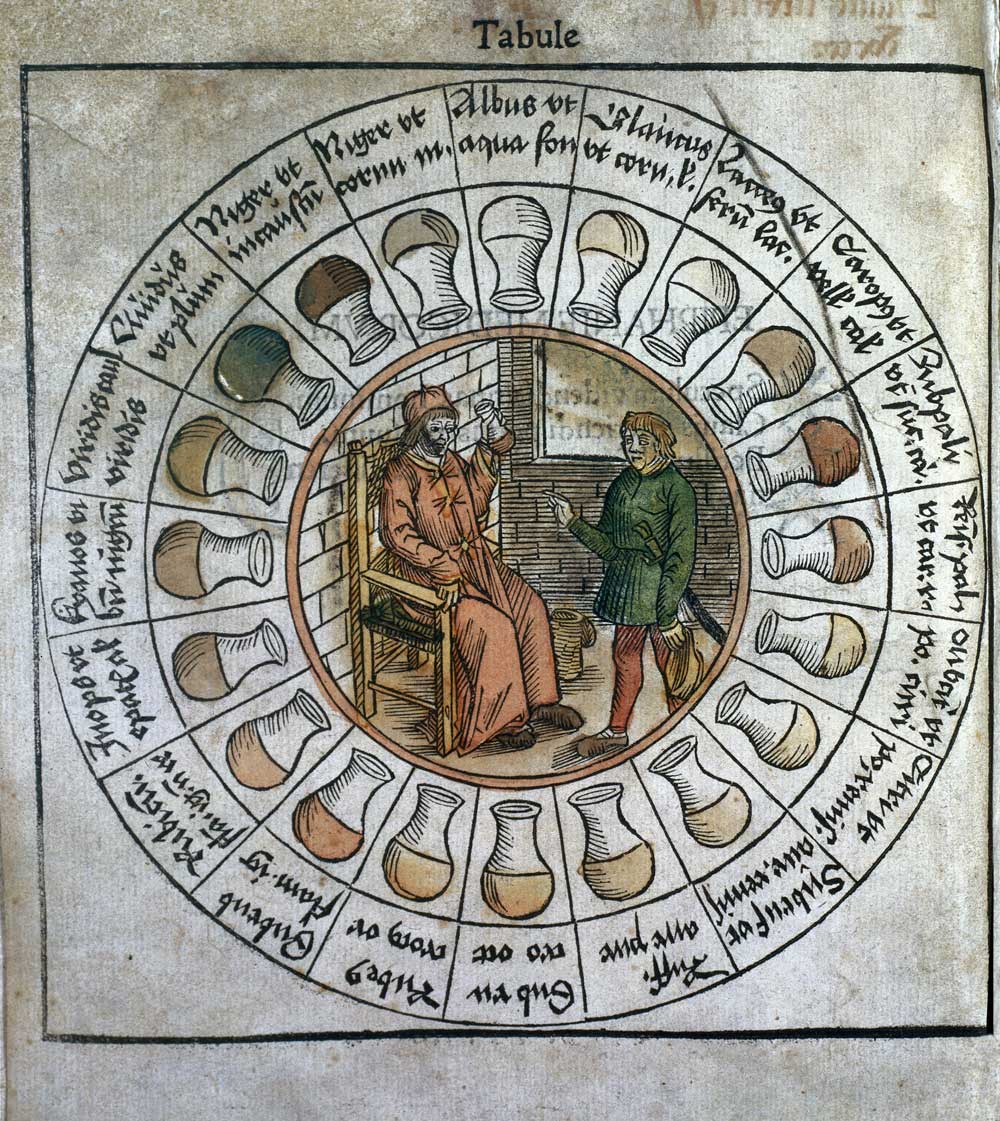
Uroscopy, the diagnosis of disease by visual examination of the urine, can be regarded as one of the oldest medical diagnostic tools. Its roots can be traced back to Sumerian and Babylonian medicine, more than 4000 years ago. From the Middle Ages, the importance gained rapidly, beginning with the Byzantine physicians. Johannes Zacharias Actuarius (1275-1328), in his manuscript, De Urinis Libri Septem, gave detailed instruction on how urine should be collected.
From the 13th-14th century onwards, several treatises on the judgement of the urine were published all over Europe. Soon, these treatises began to be published in the vernacular and served the physicians as guidebooks when consulting their patients. The examination of the “water” had an indispensable function and the club-shaped urinal known as “matula” (uroscopy flask) became the guild symbol of the physician.
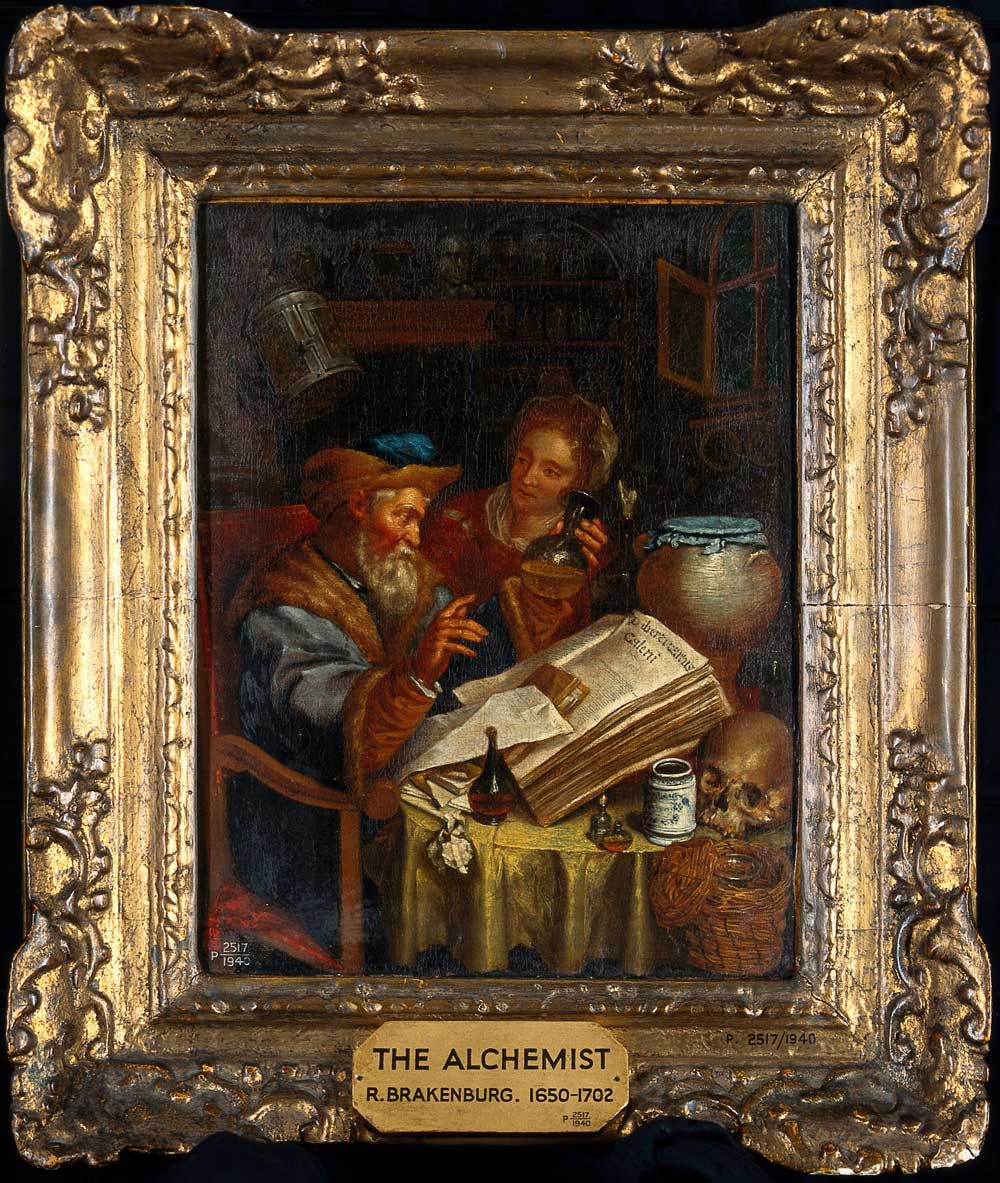
Within academic societies of urology, the doctor performing uroscopy became a popular image for logos. The AUA has used this image since a 1937 presentation on hematuria, as did the DGU from its beginnings with a more ancient motif (Hippocrates doing uroscopy).
Today physical, chemical and biological tests of urine are the base in testing kidney diseases.



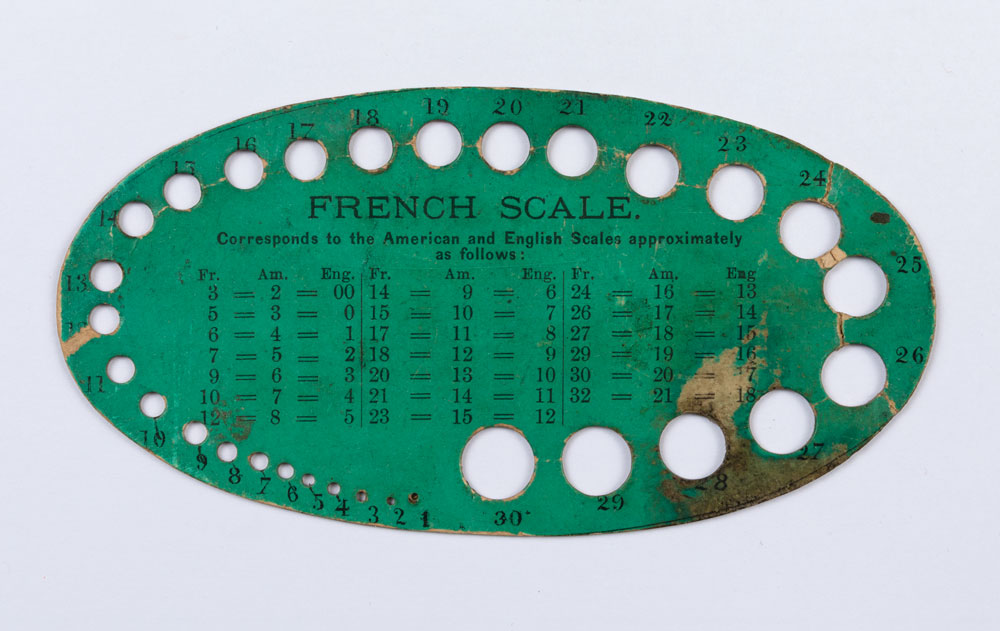
On a daily basis, the French scale is employed as a unit of measure to describe the diameter of needles, sounds, catheters, urethral instruments, and fiber optic bundles. Yet few know who gave us the French scale. That person is Joseph-Frédéric-Benoît Charrière, a Swiss-born craftsman who became the most renowned surgical instrument manufacturer of his day.
Charrière introduced the scale in 1842 and originally called the French scale the “filière Charrière,” or the Charrière gauge. Charrière recounted its origins in a catalogue prepared for the Paris Industrial Exposition of 1849:
Many physicians have encountered problems obtaining sounds and bougies of a diameter that they wanted. To rectify this situation, it was essential to establish a standard gauge which, by its divisions and the perfect regularity of its graduation, might constitute a sure and certain guide. I fashioned a standard measure that meets these criteria; the gauge is pierced by thirty holes, which served to take the measure of sounds and bougies. Each hole corresponds to two numbers. The former indicates the place in the sequence of holes; the latter indicates the diameter of the sound. One may see that I divided my gauge in thirds of a millimeter. This division fulfills, I think, all indications.

Just one year after cocaine’s 1884 introduction as a local anesthetic, syringes were first used to administer “spinal” anesthesia. Over the next few decades, despite its superior safety to etherization for high-risk patients, there was a marked reluctance to use regional anesthesia in urologic surgery.
During this period, the relative efficacy and toxicity of each agent and the efficacy and risks of each injection site, all in relation to specific types of surgery, were discovered. Many new local anesthetic drugs were also introduced, including the “new cocaine” (procaine hydrochloride, or Novocain), synthesized in 1904. An important factor that slowed adoption of the method was unintended diffusion of the agent towards the brain or a “high spinal,” which could include falling blood pressure and failing respiration. These problems were minimized or remedied by the control of injectate baricity (density) and of patient positioning, the addition of central nervous system and cardiorespiratory stimulants, and the use of positive-pressure ventilation.
Gaston Labat, M.D. published his own classic textbook, Regional Anesthesia,Its Technic and Clinical Application, in 1922. This introduced the Labat Regional Anesthesia Outfit. The outfit contains a syringe and needles specifically designed for conducting regional anesthesia, together with a metal sterilizing tray. The kit shown here was made by the Anglo-French Drug Company of New York. The Labat syringe and needles continued to be manufactured through the 1960s.
In 1923, Dr. Labat founded the American Society for Regional Anesthesia (ASRA). Later re-founded and then renamed as the American Society for Regional Anesthesia and Pain Medicine, ASRA is now the leading professional organization for these subspecialties. Since 1977, ASRA has presented annually the Labat Award for an outstanding contribution to one of these fields.


The history of bladder stone removal is both long and stomach-churning. The earliest known bladder stone was found in the pelvis of a mummy at El-Amrah in Egypt; it is estimated to be 5,000 - 7,000 years old. Bladder stones even managed to find their way into the Hippocratic Oath: physicians must swear that they “will not cut for the stone, but will leave this to be done by practitioners of this work.”
The problem of a stone too large to be pulled through the incision was a frequent encounter during lithotomies, and was especially troublesome because these types of surgeries were meant to be kept as short and as non-invasive as possible in order to avoid common and dangerous complications. At the beginning of the 19th century, fragmenting or crushing instruments were introduced to reduce the size of the stones. These “lithotrites” or “lithoclasts” almost immediately reduced the mortality rate oflithotomies from 25% to 2.4%.
A modern lithotomy is much less frightening than it once was. Technology has advanced so that incisions are no longer needed to treat a bladder stone — a bladder calculus can be visualized via a cystoscope and broken up using a laser. This dramatically reduces the pain felt by the patient and his or her recovery time.


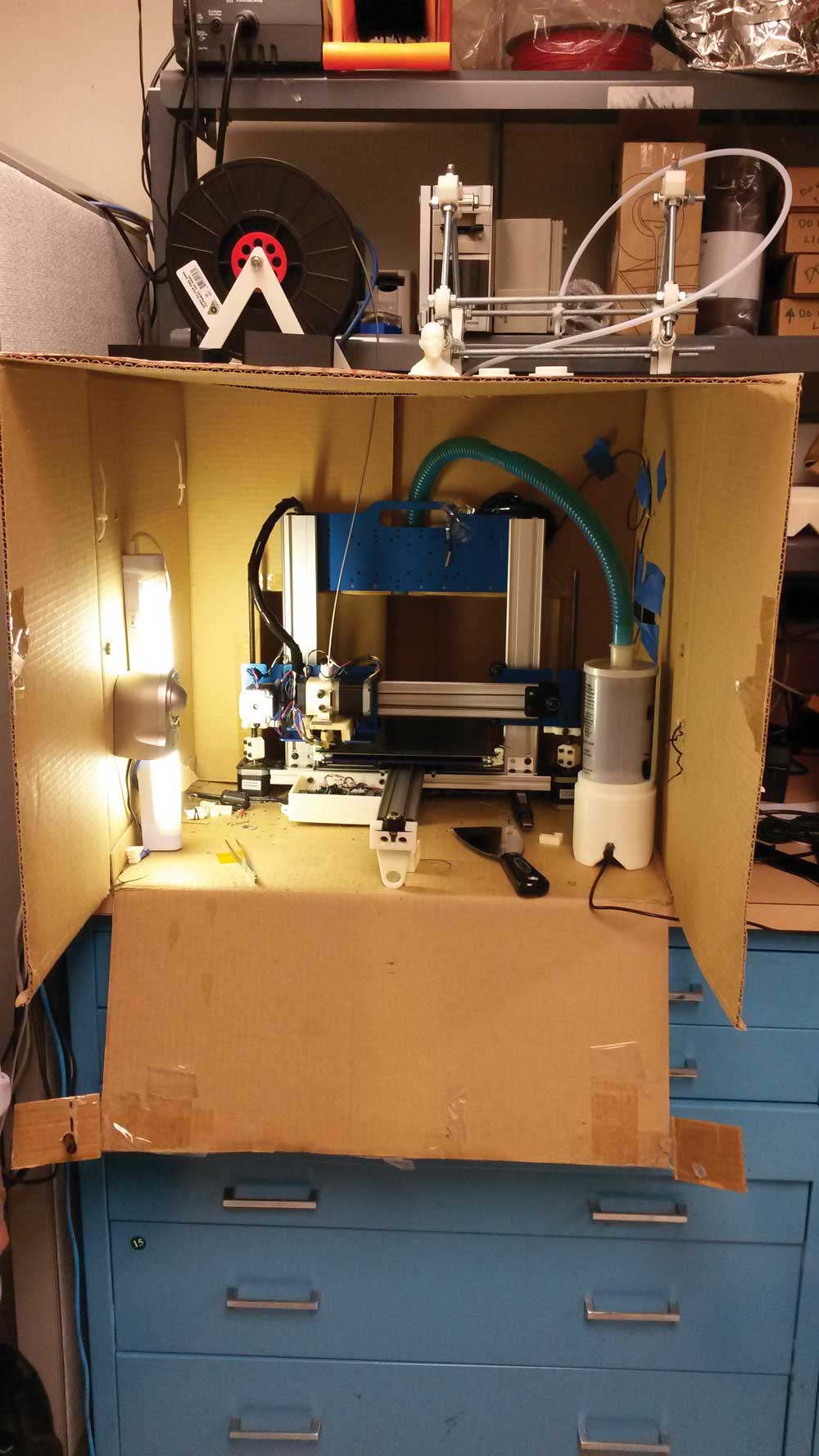
First, you’d have to make sure that the MRI results matched to a prostatectomy specimen.
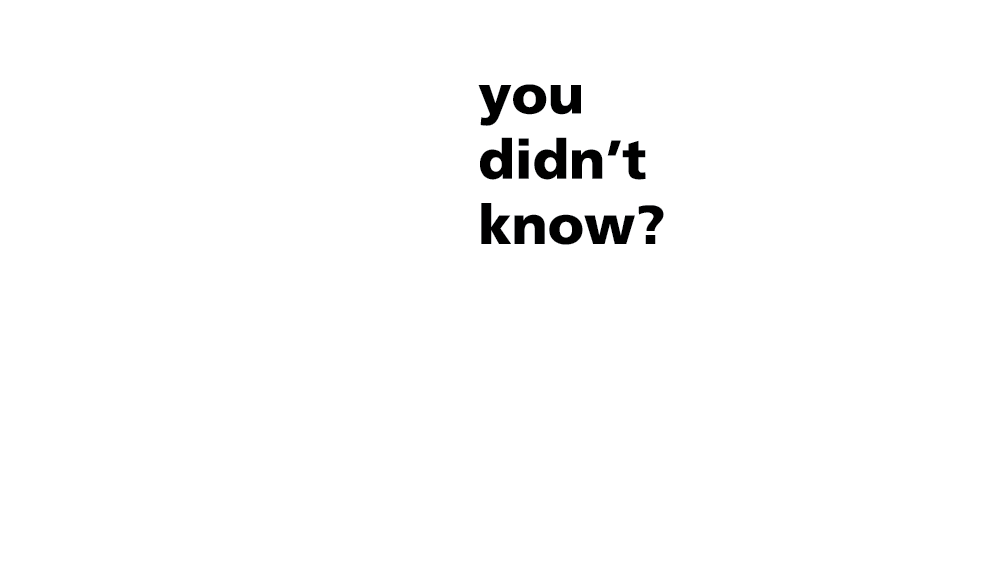
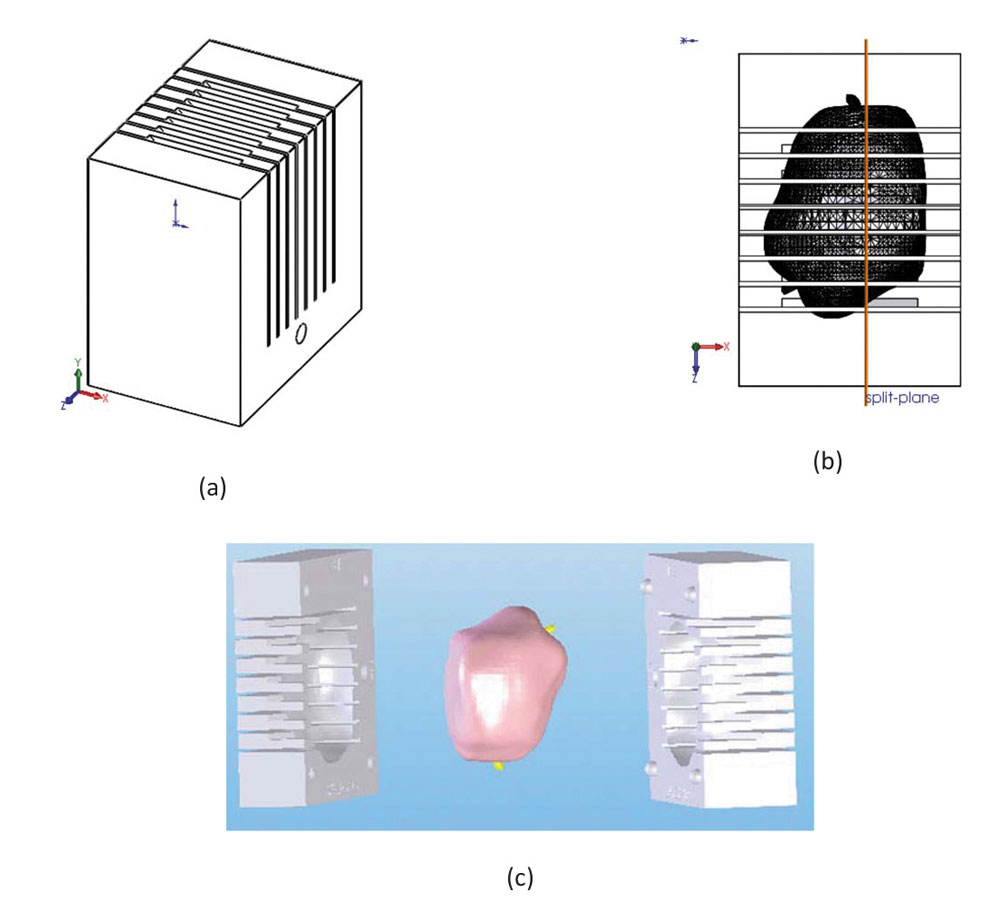
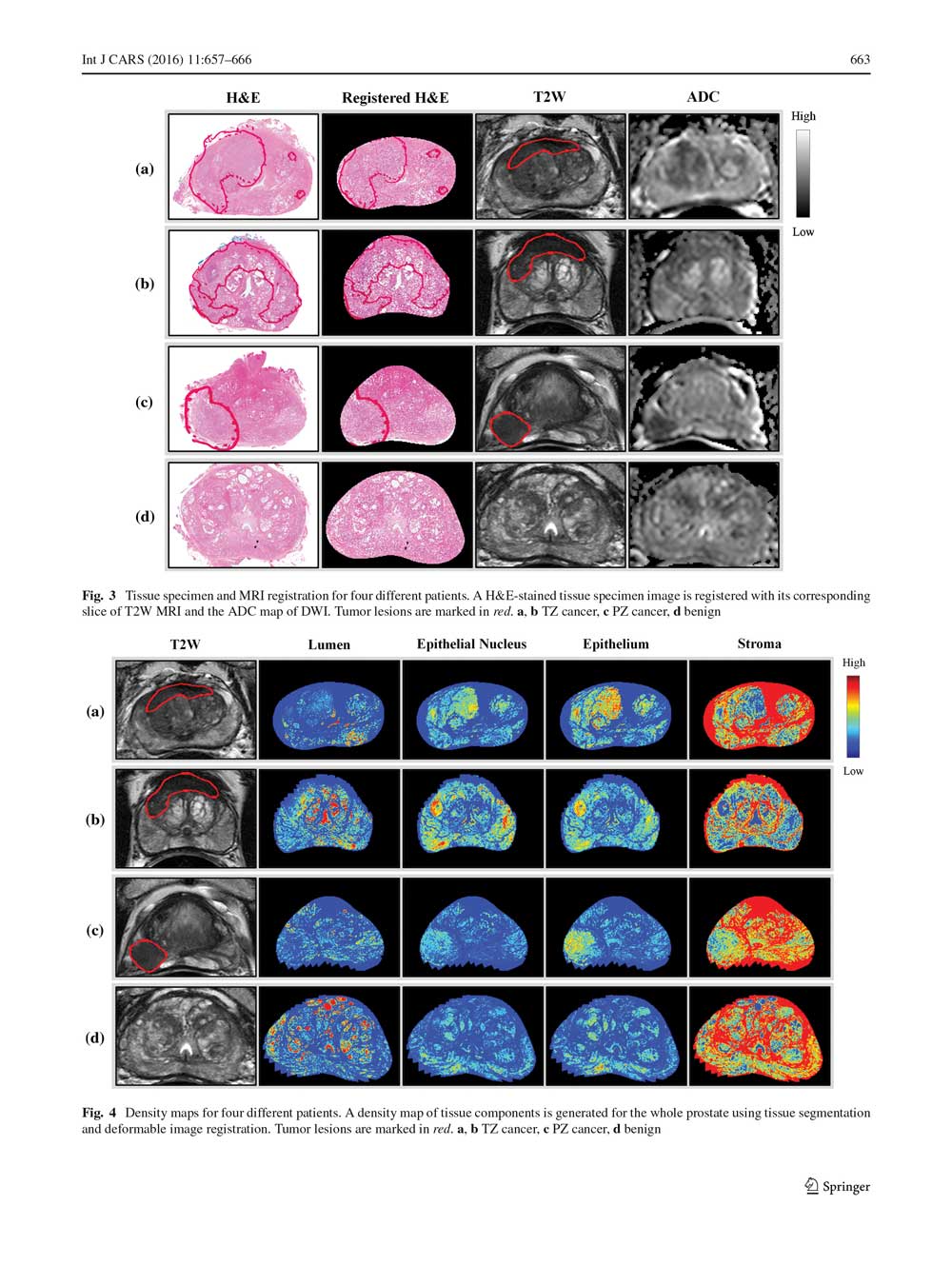
A group at the National Cancer Institute’s Center for Cancer Research (CCR) uses 3D printing to create patient-specific prostate molds from MRIs. The mold is printed prior to surgery; after the prostate is removed, it fits into the mold and, because the prostate is oriented and shaped just as it is in the MRI, histopathology sections can be cut so they can be accurately compared to MRI.
The modern management of primary nocturnal enuresis involves a history and physical examination. The history includes details of deep sleep, urinary tract infections, constipation, daytime wetting, encopresis, medications for other conditions, fluid and caffeine intake, and family psychosocial dynamics. The physical examination includes a neurological examination, evidence of constipation, perineal and/or genita lirritation, external spinal examination, and evidence of sexual molestation. When no underlying cause is identified, modern treatment, when indicated by the child and/or his family, involves using a conditioning device or enuresis alarm. This may be combined with careful controlled pharmacotherapy with Desmopressin (DDAVP) and sometimes Oxybutynin (Ditropan).
In the recent past, medications such as Imipramine (Tofranil), Amphetamine, Tincture of Belladonna, Propantheline (Pro-Banthine), and Posterior Pituitary Snuff were tried.
The first use of mice to treat enuresis dates back to Pliny the Elder (79CE): The incontinence of urine in infants is checked by giving boiled mice in their food.
Thomas Lupton (1579) wrote:
A flayne Mouse, or made in powder and drunk at one tyme, doeth perfectly help such as cannot holde or keepe their water: especially, if it be used three days in this order. This is verie trye and often puruved.
Additional animal parts have been recommended to treat enuresis. Thomas Phair (1545) wrote in the first British textbook on childhood disorders: Take the wesande of a cocke and pluck it, tha brenne it in pouder and vse it twyse or thryse a daye. The stones of a hedge hogge poudered is of the same vertue. Item the clawes of a goate...
The German born Abraham Jacobi, considered to be the father of American Pediatrics, made suppositories of sheep fat mixed with strychnine for the management of enuresis (1891). Jacobi, the only foreign-born President of the American Medical Association, also believed that masturbation was a cause of nocturnal enuresis.
Toads were reported to be the precursor to the enuresis alarm. In western Nigeria, a toad is tied to the penis. When the toad gets wet, it croaks and awakens the boy.
Mice, toads, and animal parts represent artifacts that describe unproven methods to treat enuresis. A double blind study on the use of Mouse Toast to treat enuresis has not been reported.